Oral gonorrhea is an infection caused by the sexually transmitted bacterium Neisseria gonorrhoeae. Many people don’t show symptoms, so it often goes undiagnosed and untreated. Understanding this infection’s symptoms, how it spreads, and its treatment options is crucial for sexually active individuals. This guide will provide you with comprehensive information on managing and preventing oral gonorrhea.
Key Takeaways
- Oral gonorrhea, caused by Neisseria gonorrhoeae, is often asymptomatic, making awareness and prevention crucial for sexually active individuals.
- Diagnosis of oral gonorrhea requires thorough testing due to symptom overlap with other throat infections such as strep throat, particularly for those under 25.
- Preventive measures including consistent condom use, dental dams, and open communication about sexual health are vital in reducing the transmission of oral gonorrhea.
- Untreated gonorrhea infection can lead to serious health problems in both males and females
What Is Oral Gonorrhea?

Oral gonorrhea bacterial infection, caused by the bacterium Neisseria gonorrhoeae, is a sexually transmitted infection that can affect the throat. This infection is primarily transmitted through vaginal, anal, and oral sexual activities, making it a concern for sexually active individuals.
Gonorrhea can be transmitted even without complete penetration during sexual encounters. Moreover, the bacterium responsible for oral gonorrhea can lead to throat infections, which may often present no symptoms, making it easy for the infection to go unnoticed and untreated.
Infected individuals can spread oral gonorrhea even without symptoms. This silent transmission highlights the need for awareness and preventive measures to protect everyone.
Common Symptoms of Throat Gonorrhea
Oral gonorrhea often flies under the radar because it is frequently asymptomatic. Many individuals harbor the infection without any apparent signs, contributing to its unnoticed spread. When symptoms do appear, they can be easily mistaken for more common throat infections.
Common symptoms of throat gonorrhea include:
- a persistent sore throat
- difficulty swallowing
- swollen lymph nodes
- fever
These symptoms can be misleading, as they overlap with those of other throat infections. However, unlike strep throat, oral gonorrhea may not always present with noticeable symptoms even when an active infection is present.
Differentiating between these infections is crucial. Both strep throat and oral gonorrhea can cause a sore throat and swollen lymph nodes.
How Oral Gonorrhea Spreads
Oral gonorrhea is primarily transmitted through sexual contact, particularly via unprotected oral sex with an infected person. Engaging in such activities without protection significantly increases the risk of contracting this infection. Although oral gonorrhea spreads mainly through oral sex, there is some evidence that intimate kissing with an infected person can also transmit the infection.
Individuals with multiple sexual partners are at a higher risk of contracting oral gonorrhea due to increased exposure. It is a misconception that casual contact, like kissing or sharing utensils, can spread gonorrhea—this differentiates it from other infections that spread via respiratory droplets and sexually transmitted disease.
Knowing these transmission routes helps adopt safer sexual practices to prevent gonorrhea.
Diagnosing Throat Gonorrhea
Diagnosing throat gonorrhea involves a comprehensive approach. A medical history review and physical examination are the first steps, followed by throat swab testing for Neisseria gonorrhoeae. This testing is essential because the symptoms can mimic other common infections like the common cold.
For accurate diagnosis, samples should be taken from both urogenital and extragenital sites based on individual sexual behavior. Regular sti testing is particularly important for individuals under 25 years old, who are at a higher risk for gonorrhea. Additionally, testing for other sexually transmitted infections may be recommended when diagnosing throat gonorrhea, as co-infections are possible.
Routine screening is vital for those at high risk, particularly individuals with multiple sexual partners. This proactive approach aids in early detection and treatment, which helps to prevent sexually transmitted infections and the infection’s spread.
Treatment Options for Oral Gonorrhea

Treating oral gonorrhea typically involves antibiotics. A common regimen includes a single dose of ceftriaxone and a seven-day course of oral azithromycin. Other antibiotics like cefixime, cefotaxime, and spectinomycin may also be used in certain cases. Completing the full course of antibiotics ensures the infection is fully cleared and prevents recurrence.
Patients often experience improvement in symptoms within a couple of days after starting antibiotic treatment. However, individuals diagnosed with oral gonorrhea should avoid oral sex until completely cured and must inform their recent sexual partners. Notifying and encouraging partners to seek treatment can lead to better health outcomes and reduce the risk of re-infection.
Resistance to other antibiotics can make treatment more challenging, impacting the likelihood of recurrence. Therefore, adherence to the prescribed treatment regimen and partner notification are pivotal in managing and preventing the spread of oral gonorrhea.
Preventing Oral Gonorrhea
Prevention is always better than cure. Consistent use of condoms during sexual activities is crucial to minimize the risk of gonorrhea. Additionally, using dental dams during oral sex can help protect against throat gonorrhea and support disease control.
Practicing safe sex, including regular testing, is an effective way to prevent the spread of throat gonorrhea. Open discussions about sexual health with partners can significantly reduce the risk of gonorrhea transmission. By adopting these preventive measures, individuals can protect themselves and their partners from this infection.
Complications of Untreated Gonorrhea
Untreated gonorrhea can travel through your bloodstream and lead to significant complications in both men and women, affecting their reproductive health and overall well-being. Here are the primary complications:
In Women:
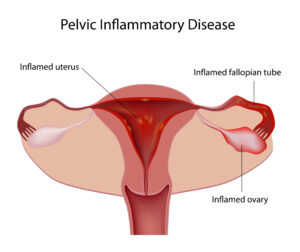
- Pelvic Inflammatory Disease (PID): An infection of the uterus, fallopian tubes, or ovaries.
- Infertility: Damage to the fallopian tubes can block or scar them, preventing pregnancy.
- Chronic Pain: Persistent pelvic pain due to internal scarring or ongoing inflammation.
- Disseminated Gonococcal Infection (DGI): If the bacteria spread to the bloodstream, it can cause joint pain, skin lesions, fever, and other systemic symptoms.
- Increased Risk of HIV: Gonorrhea can increase susceptibility to contracting or transmitting HIV.
- Complications During Pregnancy: Untreated gonorrhea can result in premature birth, low birth weight, or infection of the newborn’s eyes (neonatal conjunctivitis) during delivery.
In Men:
- Epididymitis: Inflammation of the epididymis (a tube that stores sperm) can cause pain, swelling, and infertility if untreated.
- Prostatitis: Infection of the prostate gland leading to pain, difficulty urinating, and sexual dysfunction.
- Urethral Strictures: Scarring in the urethra can cause narrowing, making it difficult to urinate.
- Infertility: Chronic infections can impair sperm production or delivery.
- Increase Risk of HIV: Similar to women, untreated gonorrhea raises the risk of HIV transmission.
Shared Complications:
- Spread to Other Organs: Infections in the throat, rectum, or eyes can cause localized discomfort or more severe systemic issues if untreated.
- Septic Arthritis: Gonorrhea can infect joints, leading to pain, swelling, and immobility.
Oral Gonorrhea vs. Other Throat Infections
When symptoms develop from oral gonorrhea infection, they can be indistinguishable from strep throat symptoms. Oral gonorrhea may sometimes present symptoms that resemble those of other throat infections, making diagnosis challenging.
However, oral gonorrhea can be differentiated from strep throat based on the different bacterial causes, along with higher fever and more severe symptoms in strep throat. Understanding these differences can help in seeking the appropriate medical care and treatment.
When to See a Doctor or Seek Medical Attention
If you experience symptoms or have had unprotected sex or unprotected oral sex with an infected partner, you should seek medical attention. Early diagnosis and treatment are crucial for managing the infection and preventing its spread.
Immediate medical help is necessary if there is a severe sore throat or difficulty swallowing alongside other symptoms. If symptoms worsen or new symptoms arise after the initial infection, it’s crucial to consult a healthcare provider.
Notifying your healthcare provider and potentially your partner if you believe you have been exposed to gonorrhea is essential for effective management.
Communicating With Partners About Oral Gonorrhea
Informing sexual partners about oral gonorrhea is crucial for their health and to prevent further spread. Open communication about sexually transmitted diseases helps prevent the spread of infections and promotes healthier sexual practices.
Effective communication about STIs can reduce stigma and encourage healthier sexual practices among individuals. Confidentiality and sensitivity are important when discussing STI status to ensure partners feel safe to engage in open dialogue.
Partner notification is a critical strategy aimed at informing sexual partners about potential exposure to STIs.
Likelihood of Recurrence
The likelihood of recurrence of oral gonorrhea is influenced by several factors, including the effectiveness of treatment, immune system health, and sexual behavior. A robust immune system can lower the likelihood of recurring gonorrhea infections. Engaging in high-risk sexual behaviors increases the chances of reinfection with gonorrhea.
To reduce the risk of recurrence, it is important to practice safe sex and get tested regularly. Individuals should abstain from sexual activity until cured and complete the full course of antibiotics to avoid re-infection.
Summary
Understanding oral gonorrhea involves knowing its symptoms, transmission routes, and preventive measures. Early diagnosis and treatment are crucial in managing this infection and preventing complications. Practicing safe sex and maintaining open communication with partners are essential steps in protecting yourself and others. Stay informed, stay safe, and prioritize your sexual health.
FAQs
How is oral gonorrhea transmitted?
Oral gonorrhea is primarily transmitted through unprotected vaginal, anal, and oral sexual activities. Taking precautions during intimate contact is essential to prevent transmission.
What are the common symptoms of throat gonorrhea?
Common symptoms of throat gonorrhea include a sore throat, difficulty swallowing, and swollen lymph nodes, although many cases may present without noticeable symptoms. This asymptomatic nature can complicate diagnosis and treatment.
What other sexually transmitted infections can give you a sore throat?
Infections like chlamydia and herpes can also cause a sore throat when transmitted through oral sex. They may present with symptoms similar to common throat infections.
Can you get oral gonorrhea through oral sex?
Oral gonorrhea is transmitted when Neisseria gonorrhoeae bacteria spread to the throat through oral-genital contact, oral-anal contact, or exposure to infected bodily fluids such as semen, vaginal fluids, or rectal secretions.
How is throat gonorrhea diagnosed?
Throat gonorrhea is diagnosed through a review of medical history, physical examination, and by conducting throat swab tests specifically for Neisseria gonorrhoeae. Regular testing is essential, particularly for those at higher risk.
What are the treatment options for oral gonorrhea?
The most effective treatment for oral gonorrhea is a combination of a single dose of ceftriaxone and a seven-day course of oral azithromycin. It is crucial to complete the entire course and inform recent sexual partners for proper management.
How can oral gonorrhea be prevented?
Oral gonorrhea can be effectively prevented by consistently using condoms and dental dams during oral sex, practicing safe sexual habits, and engaging in regular testing. Additionally, maintaining open communication with sexual partners is essential for prevention.
What Sexually transmitted disease most resembles oral gonorrhea?
Other sexually transmitted infections like chlamydia and herpes can also present with throat symptoms when transmitted through oral sex. Accurate diagnosis through testing is essential to differentiate between these infections and ensure appropriate treatment.
Does throat gonorrhea go away on its own?
No, throat gonorrhea does not go away on its own. Without appropriate treatment, the infection can persist and potentially lead to more severe health complications. It is crucial to seek medical attention and follow the prescribed antibiotic regimen to ensure the infection is fully cleared.
Sources:
Healthline: How to Identify, Treat, and Prevent Oral Gonorrhea
CDC: Gonococcal Infections Among Adolescents and Adults