When you find out your partner has herpes you can feel like a whirlwind of emotions. You might be surprised, worried, or even confused. But know that herpes is a very common condition and it doesn’t have to define your relationship. With understanding, open communication, and a bit of education you can navigate this together. Many couples have healthy, happy relationships with an HSV diagnosis.
What is Herpes Simples Virus (HSV)?
Herpes simplex virus (HSV) comes in two forms: herpes simplex virus type 1 (HSV-1) and herpes simplex virus type 2 (HSV-2). Herpes simplex virus type 1 is more commonly associated with cold sores around the mouth, while herpes simplex virus type 2 is primarily genital herpes. But both can affect either area through oral or genital contact.
Herpes is very common. According to the World Health Organization (WHO), approximately two-thirds of the global population under 50 have HSV-1, and 520 million people aged 15-49 have HSV-2. Knowing these numbers can help you see you and your partner are not alone.
Symptoms and Diagnosis
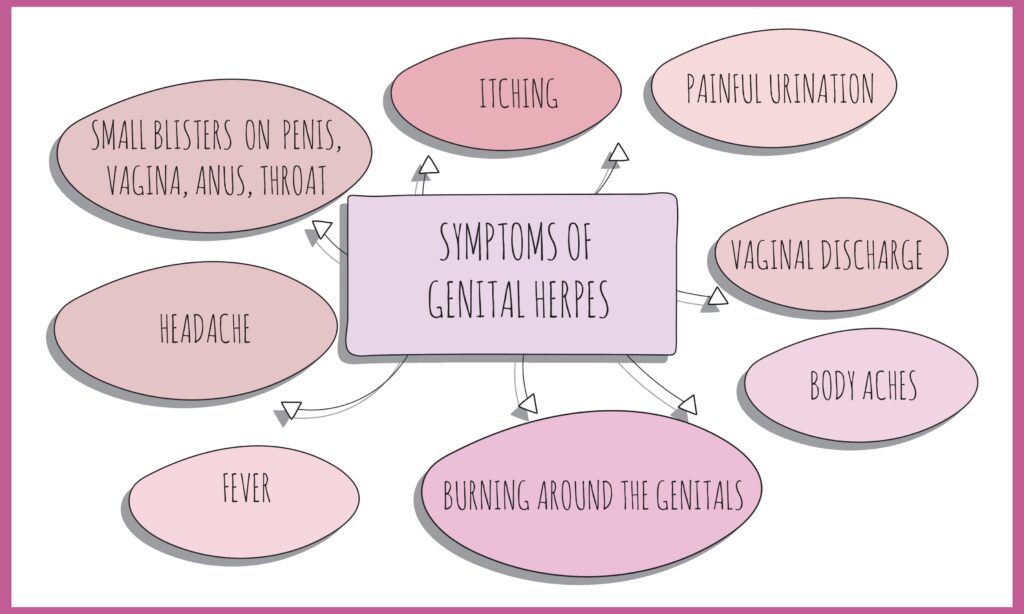
Genital herpes symptoms can vary widely, and sometimes they might not be noticeable at all. The first outbreak is often the most severe and can last for several weeks. Common genital herpes symptoms include:
- Painful blisters or sores on the genitals, anus, or thighs
- Itching, burning, or tingling sensations in the genital area
- Flu-like symptoms such as fever, headache, and swollen lymph nodes
- Discharge or bleeding from the genitals
- Painful urination
- Genital irritation that might be mistaken for other causes such as hygiene products or grooming practices
If you or your partner notice any of these symptoms, it’s important to see a doctor. They can diagnose genital herpes through a physical examination, taking a sample of fluid from a sore, or conducting a blood test to detect the herpes simplex virus. Early diagnosis and treatment can help manage the symptoms and reduce the risk of transmission.
How is Genital Herpes Transmitted?
Genital herpes is transmitted through any form of contact with an infected partner, usually during an outbreak when sores are present. But it can also be transmitted when no symptoms are present, called asymptomatic shedding. So even when there are no visible symptoms precautions are important to prevent transmission.
Complications and Risks
Living with genital herpes has several complications and risks so it’s important to manage it well. These include:
- Recurrent Outbreaks: Genital herpes can cause recurrent outbreaks which can be triggered by stress, fatigue or hormonal changes. These recurrent outbreaks can be managed with antiviral meds and lifestyle changes.
- Increased Risk of HIV Transmission: People with genital herpes are more prone to HIV infection. The sores from herpes can be an entry point for the HIV virus so it’s important to take precautions.
- Neonatal Herpes: Pregnant women with genital herpes can pass the virus to their baby during delivery and it can cause serious health complications for the newborn. Pregnant women with herpes should discuss their condition with their doctor.
- Meningitis and Encephalitis: In rare cases genital herpes can cause meningitis (inflammation of the membranes surrounding the brain and spinal cord) or encephalitis (inflammation of the brain). Seek medical attention immediately.
- Psychological Distress: The emotional impact of living with genital herpes can be huge, leading to anxiety, depression and feeling isolated. Seeking help from a therapist or joining a support group can be helpful.
- Genital Herpes Sore Risks: Knowing the risks of genital herpes sores is important. These sores can cause complications like increased susceptibility to other infections and huge emotional distress.
Knowing these risks and complications will help you and your partner to manage genital herpes and your overall health and well-being.
The Stigma
Despite how common herpes is, it’s surrounded by unnecessary stigma. This stigma can lead to shame or fear but it’s based on misconceptions, not facts. Understanding the nature of a herpes infection can help reduce stigma and promote better communication. Education is key to breaking down these barriers. Remember having herpes doesn’t define someone’s character or worth. Many people with herpes live normal healthy lives.
Communicate
Why Communication is Important
Open honest communication is key to building trust. Learning about your partner’s condition gives you both a chance to understand each other better. It also shows your partner you care about them and are willing to navigate through challenges together.
Conversation Tips
- Pick a quiet private place where you can talk without interruptions.
- Approach the topic with curiosity, not judgment. Remember your partner will feel vulnerable.
- Let your partner share their experience and feelings. Don’t interrupt.
Questions to Ask
- When were you diagnosed?
- How do you manage your condition?
- Have you talked to a doctor about transmission prevention?
These questions will help you understand the practical and emotional side of their diagnosis. For more tips on how to have these conversations, the American Sexual Health Association (ASHA) has resources.
How Do You Protect Yourself
Importance of STD Testing
Regular STD testing is crucial for anyone who is sexually active, especially if your partner has herpes or any other sexually transmitted infection. Testing allows for early detection and treatment, which can prevent complications and reduce the risk of transmission to others. It is important to remember that some STDs, including herpes, can be asymptomatic, meaning you might not show any symptoms but can still spread the infection.
Types of Tests
For herpes, specific blood tests can detect herpes simplex virus antibodies, which indicate a past or current infection. These tests can differentiate between HSV-1 and HSV-2, helping you understand your risk and take appropriate precautions. In addition to herpes testing, comprehensive STD panels often include tests for HIV, chlamydia, gonorrhea, syphilis, and other common infections.
When to Get Tested
Consider getting tested if you have a new sexual partner, multiple partners, or if your partner has been diagnosed with an STD. It’s also wise to get tested if you or your partner experience symptoms such as unusual discharge, sores, or flu-like symptoms. Regular testing is a proactive step in maintaining your sexual health and ensuring the well-being of your partner.
Discussing Testing with Your Partner
Openly discussing STD testing with your partner can strengthen trust and communication in your relationship. Encourage each other to get tested and share your results. This transparency can help you both make informed decisions about your sexual health and take necessary precautions.
Medication for Recurrent Outbreaks
Antiviral medications like valacyclovir or acyclovir can reduce the frequency of outbreaks and the risk of passing herpes to a partner. Studies show daily antiviral therapy can lower transmission rates by up to 50%. Talk to your partner about if they are taking these medications and consider talking to a healthcare provider about it.
Other Precautions
Open communication about symptoms. If your partner notices early signs of an outbreak such as tingling or redness it’s best to avoid intimate contact until symptoms go away. Recognizing early signs of herpes sores can help prevent transmission. Knowing these warning signs can help you feel more in control.
Emotional Support for Both of You
Empathy is Key
Herpes can be emotionally heavy. Your partner may feel embarrassed or fearful of being rejected. Let them know their diagnosis doesn’t change how you feel about them. Genital herpes sores can impact dating experiences, so it’s important to have open communication about outbreaks and the presence of sores. A supportive attitude can make all the difference.
Take Care of Yourself
You have your own concerns. Talking to a therapist or joining a support group can help you process your feelings and get some perspective. Websites like the Herpes Opportunity have support for individuals and couples (Herpes Opportunity Support).
Intimacy
Intimacy isn’t just physical. Explore non-sexual ways to connect like spending quality time together, sharing hobbies or having deep conversations. Focus on what makes your relationship special.
Decide
Weighing Risks and Rewards
Take some time to learn about herpes before making any big decisions about your relationship. Consider what your partner brings to your life. Many people find the benefits of their relationship outweigh the risks.
Talk to a Healthcare Provider
A healthcare provider can answer your questions and help you both figure this out. Genital herpes is classified as a sexually transmitted infection (STI), making regular testing crucial for anyone who is sexually active. Regular STD testing is a good idea for anyone who is sexually active.
FAQs
Can I get herpes simplex virus if my partner doesn’t have an outbreak?
Yes, herpes can be transmitted even when there are no sores or symptoms. This is due to asymptomatic shedding where the herpes virus is present on the skin without symptoms. The herpes virus can be transmitted even when there are no visible symptoms. Using condoms and antiviral medication can reduce the risk.
Is herpes a sign of cheating?
Not necessarily. Herpes can be dormant for years before symptoms show up. Your partner could have been infected before you even met. Approach this conversation without jumping to conclusions.
Can I still have a normal sex life with my partner?
Yes. Many couples manage herpes with open communication, safe sex, and sometimes antiviral medication. Herpes is primarily spread through sexual contact, including vaginal, anal, and oral sex, so using protection like condoms is important. Intimacy isn’t just physical and you can explore other ways to connect if needed.
Should I get tested if my partner has the herpes virus?
Yes, it’s a good idea to get tested. While standard STD panels may not include herpes, there are specific blood tests for HSV antibodies. Testing for both genital and oral herpes is important for comprehensive sexual health. Talk to your healthcare provider about testing options.
How do I support my partner?
Be kind and non-judgmental. Let your partner know their diagnosis doesn’t change how you feel about them. Encourage open communication and consider seeking support together if needed.
Should we have sex if my partner has active herpes sores?
It is strongly advised to avoid sexual contact when your partner has active herpes sores. Herpes is highly contagious during an outbreak, and engaging in sexual activity can significantly increase the risk of transmission.
Sources:
- World Health Organization – Herpes Fact Sheet
- American Sexual Health Association – Talking About Herpes
- Centers for Disease Control and Prevention – Herpes Guidelines
- Herpes Opportunity – Support and Education
- Planned Parenthood – STD Testing
